
Cancer is a malignant neoplasia marked by the uncontrolled growth of cells, often with invasion of healthy tissues locally or throughout the body.
Cancer is the second leading cause of death after cardiovascular disease. Ionizing radiation, ultraviolet light, some viruses, and drugs that damage nucleic acids may initiate the genetic lesions that result in cancers. The best-known and most widespread type of carcinogen exposure, however, is consumption of tobacco.
Prostate Cancer
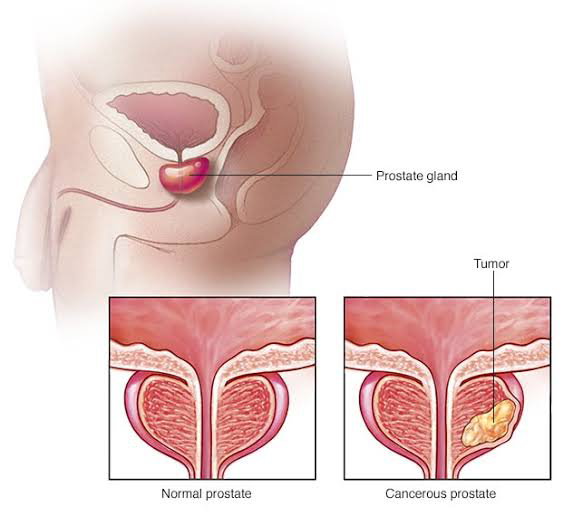
Prostate cancer is the most common type of cancer in men, it may begin with a condition called prostatic intraepithelial neoplasia (PIN), which can develop in men in their 20s. In this condition, there are microscopic changes in the size and shape of the prostate gland cells.
The more abnormal the cells look, the more likely that cancer is present. It has been noted that 50% of men have PIN by the time they are age 50.
Adenocarcinomas compose 99% of the prostate cancers. They most frequently begin in the outer portion of the posterior lobe in the glandular cells of the prostate gland. Local spread occurs to the seminal vesicles, bladder, and peritoneum.
Prostate cancer metastasizes to other sites via the hematologic and lymphatic systems, following a fairly predictable pattern. The pelvic and perivesicular lymph nodes and bones of the pelvis, sacrum, and lumbar spine are usually the first areas to be affected. Metastasis to other organs usually occurs late in the course of the disease, with the lungs, liver, and kidneys being most frequently involved.
Causes Of Prostate Cancer
The cause of prostate cancer remains unclear, but age, viruses, family history, diet, and androgens are thought to have contributing roles. Men who have an affected first- and second-degree relative have an eightfold increased risk of developing prostate cancer. A high-fat diet may alter the production of sex hormones and growth factors, increasing the risk of prostate cancer.
Environmental exposure to cadmium (an element found in cigarettes and alkaline batteries) is also considered a risk factor.
Assessment History
Ask about family history of prostate cancer, an occupational exposure to cadmium, and the usual urinary pattern. A patient may report symptoms such as urinary urgency, frequency, nocturia, dysuria, slow urinary stream, impotence, or hematuria if the disease has spread beyond the periphery of the prostate gland or if benign prostatic hypertrophy is also present. Presenting symptoms that include weight loss, back pain, anemia, and shortness of breath are often indicative of advanced or metastatic disease.
Physical Examination
Most men with early-stage prostate cancer are asymptomatic. When symptoms occur, they include ; urinary complaints( retention, urgency, frequency, nocturia, dysuria, hematuria) and back pain.. The physician palpates the prostate gland via a digital rectal examination (DRE).
A normal prostate gland feels soft, smooth, and rubbery. Early-stage prostate cancer may present as a nonraised, firm lesion with a sharp edge. An advanced lesion is often hard and stonelike with irregular borders.
A suspicious prostatic mass is further evaluated by extending the examination to the groin to look for the presence of enlarged or tender lymph nodes.
Psychosocial
Men have reported not having a rectal examination because of embarrassment. In addition, treatment for prostate cancer can be accompanied by distressful side effects, such as sexual dysfunction and urinary incontinence.
Assess the patient’s knowledge and feelings related to these issues and the presence of support systems. Note the coping strategies the patient has used in the past to manage stressors. Include the patient’s spouse or significant other in conversations.
Treatment
Treatment is determined in consultation with the patient. It depends on the overall life expectancy (How old is the patient? Does he have other diseases that will shorten his life span?) and the nature of the tumor. The steps include
- Active surveillance
- Watchful waiting (Periodic observation)
- Radical prostatectomy,
- Radiation therapy
- Hormone therapy
Active Surveillance
The goal of active surveillance is to protect quality of life during the early management of prostate cancer by delaying invasive therapy. The healthcare team closely monitors the disease, sometimes for years, with the potential of avoiding radical treatment.
Periodic Observation
Periodic observation, or “watchful waiting,” may be proposed to a patient with early-stage, less-aggressive prostate cancer. With this option, no specific treatment is given, but the progression of the disease is monitored via periodic diagnostic tests.
Large-scale clinical trials show that men who opt for conservative treatment have a slightly higher risk for death and significantly higher rate of metastasis than those who have a radical prostatectomy.
Note that men who ingest diets high in omega-3 fatty acids and low in glycemic index as well as weight loss may have slowed tumor growth and improved prognosis.
Surgical Procedure
Radical prostatectomy has been the recommended treatment option for men with middle-stage disease because of high cure rates. This procedure removes the entire prostate gland, including the prostatic capsule, the seminal vesicles, and a portion of the bladder neck.
Side Effects Of Prostatectomy
Two common side effects of prostatectomy are;
- Urinary incontinence
- Impotence
Urinary incontinence: The urinary incontinence usually resolves with time and after performing Kegel exercises, although 10% to 15% of men continue to experience incontinence 6 months after surgery.
Impotence: Impotence occurs in 85% to 90% of patients. All men who undergo radical prostatectomy lack emission and ejaculation because of the removal of the seminal vesicles and transection of the vas deferens.
A newer surgical techniques (nerve-sparing prostatectomy) preserves continence in most men and erectile function in selected cases. Cryosurgery (cryoablation of the prostate) with liquid nitrogen is less invasive and may be associated with fewer long-term consequences (impotence and incontinence). Both techniques are under study for their long-term outcomes.
Transurethral resection of the prostate (TURP) may be recommended for men with more advanced disease, especially if it is accompanied by symptoms of bladder outlet obstruction.
This procedure is not a curative surgical technique for prostate cancer but does remove excess prostatic tissue that is obstructing the flow of urine through the urethra. The incidence of impotence following TURP is rare, although retrograde ejaculation (passage of seminal fluid back into the bladder) almost always occurs because of the destruction of the internal bladder sphincter during the procedure.
Many men equate ejaculation with normal sexual functioning, and to some, the loss of the ejaculatory sensation may be confused with the loss of sexual interest or potency.
Also, a bilateral orchiectomy may be done to eliminate the source of the androgens since 85% of prostatic cancer is related to androgens. All patients return from surgery with a large-lumen, three-way Foley catheter. The large lumen of the catheter and the large volume in the balloon (30 mL) help splint the urethral anastomosis and maintain hemostasis.
Blood-tinged urine is common for several days after surgery, but dark red urine may indicate hemorrhage. If continuous urinary drainage is used, maintain the flow rate to keep the urine light pink to yellow in color and free from clots, but avoid overdistention of the bladder.
Antispasmodics may be ordered for bladder spasms. Anticholinergic and antispasmodic drugs may also be prescribed to help relieve urinary incontinence after the Foley catheter is removed. Because of the close proximity of the rectum and the operative site, trauma to the rectum should be avoided as a means of preventing hemorrhage.
Stool softeners and a low-residue diet are usually ordered to limit straining with a bowel movement. Rectal tubes, enemas, and rectal thermometers should not be used.
Radiation Therapy
Both external beam radiotherapy and internal implant (brachytherapy) are used in the treatment of prostate cancer. Radiation therapy is also used in areas of bone metastasis.
The goal in extensive disease is palliation: Reduce the size of the prostate gland and relieve bone pain.
Brachytherapy involving the permanent (iodine-125 or gold-198) or temporary (iridium-192) placement of radioactive isotopes can be used alone or in combination with external radiation therapy.
Patients who receive permanently placed radioisotopes are hospitalized for as long as the radiation source is considered a danger to persons around them.
The principles of time, distance, and shielding need to be implemented. Care needs to be exerted so that the radioisotope does not become dislodged. Dressings and bed linens need to be checked by the radiation therapy department before these items are removed from the patient’s room.
Hormonal Therapy.
Medication choices for hormone therapy include luteinizing hormone-releasing hormone analogue, androgen antagonists, and gonadotropic-releasing hormone agonists.




Leave a Reply